The phenomenon of doctors’ illegible handwriting has long been a subject of curiosity and concern within the medical community. This issue, while often joked about, carries significant implications for patient care, prescription accuracy, and overall healthcare efficiency.
One of the primary reasons behind this enigma is the demanding nature of a physician’s job. Doctors are often pressed for time, rushing from one patient to another, and scribbling notes or prescriptions in haste. In the midst of such a hectic environment, the legibility of their handwriting can inadvertently suffer.
Moreover, the traditional medical education system may not emphasize penmanship as rigorously as other skills, such as diagnosis and treatment protocols. Consequently, many physicians may not prioritize developing clear and readable handwriting during their training.
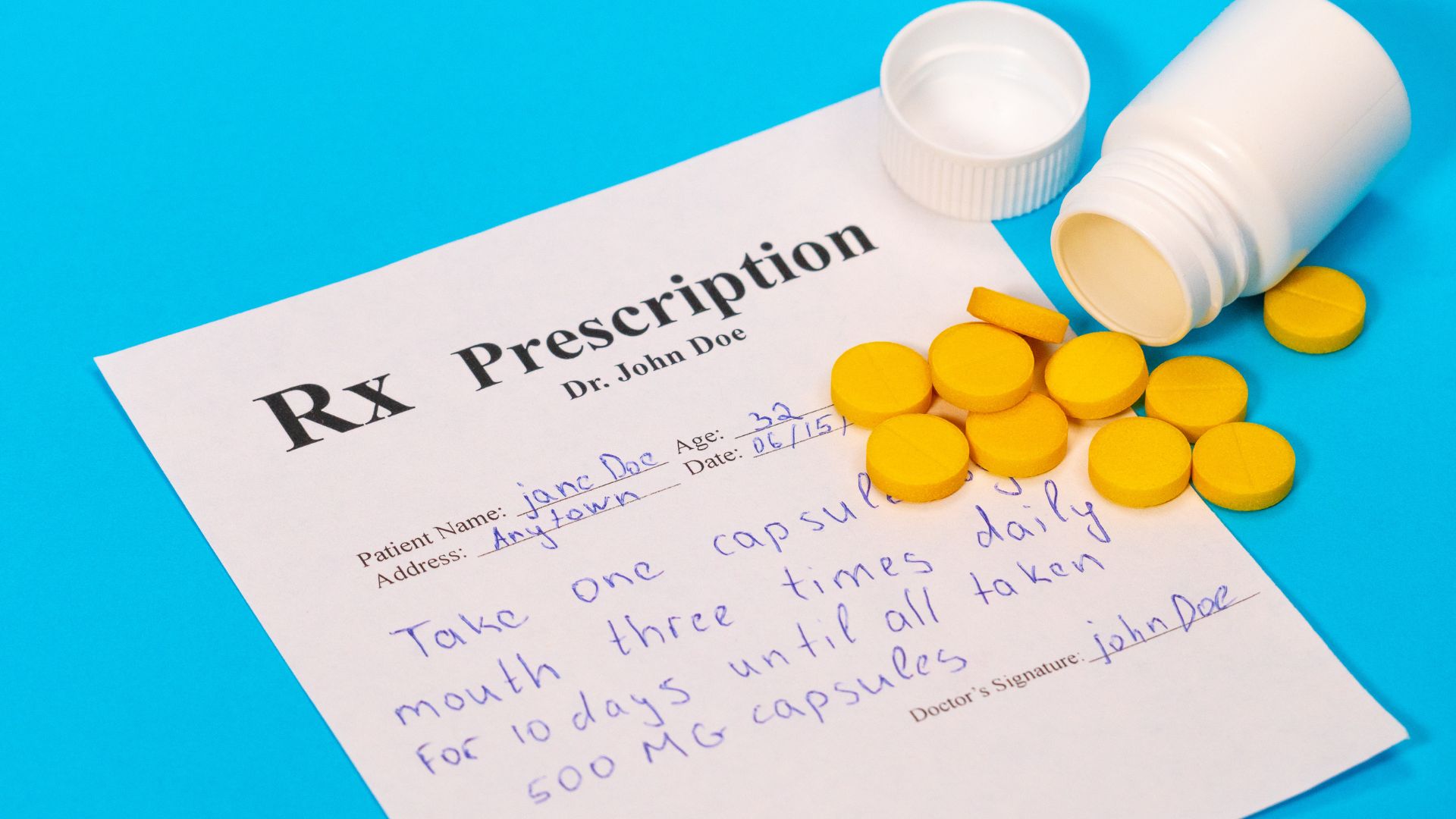
Another contributing factor is the complexity of medical terminology and abbreviations. Doctors frequently use shorthand and specialized terms in their notes and prescriptions, which may be unfamiliar to those outside the medical profession. This can further obscure the meaning of their handwriting, leading to misinterpretation and errors.
Despite advancements in electronic health records and digital prescribing systems, some healthcare facilities still rely on handwritten notes and prescriptions. While technology has the potential to mitigate this issue, its adoption varies widely across different healthcare settings and regions.
Addressing the issue of doctors’ poor handwriting requires a multi-faceted approach. Medical schools could consider incorporating handwriting improvement programs into their curriculum, emphasizing the importance of clear communication in patient care. Healthcare institutions could also invest in electronic medical records systems to minimize the reliance on handwritten documentation.
Ultimately, ensuring legible handwriting among healthcare professionals is essential for maintaining patient safety and quality of care. By acknowledging and addressing this longstanding issue, the medical community can strive towards enhancing clarity, accuracy, and efficiency in healthcare delivery.